导读
2021年10月20日,欧洲临床营养与代谢协会(European Society for Clinical Nutrition and
Metabolism, ESPEN)在其官方杂志Clinical Nutrition上在线发布了住院患者膳食营养指南(ESPEN guideline on hospital nutrition),这是ESPEN成立以来有关膳食营养的第一个指南。该指南主要依据循证医学证据对住院患者膳食营养管理提出56条推荐意见,旨在规范住院患者的膳食营养管理,使医院提供的膳食符合住院患者营养状况,充分发挥医生、护士、营养师等在住院患者膳食营养管理中的关键作用,提高膳食营养的有效性和安全性,并降低营养不良及其相关并发症的发生风险。
复旦大学附属中山医院临床营养团队第一时间将此指南翻译成文,供国内同行学习、交流,为我国的住院患者膳食营养管理提供参考。
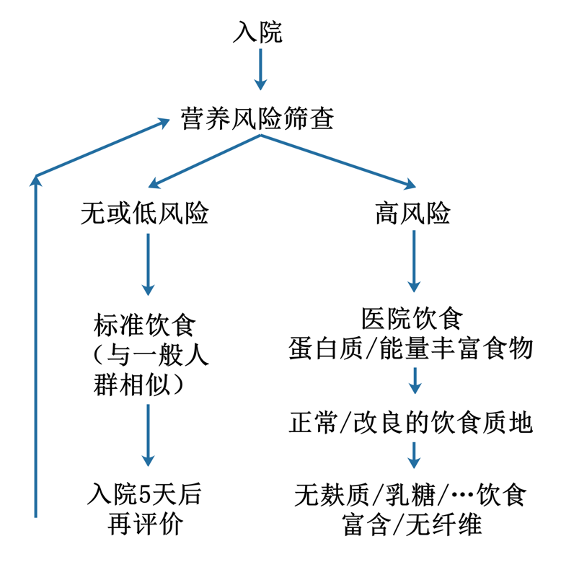
图1. ESPEN住院患者膳食营养管理流程
一、总则
推荐1
Each hospital, rehabilitation center, and nursing home should have a list
of available diets visible for patients and personnel. Grade of recommendation
GPP – strong consensus (96.5% agreement)
每家医院、康复中心和疗养院都应该为患者和工作人员提供一个可见的饮食清单。推荐等级GPP-强烈同意(96.5%)
推荐2
Each hospital shall have a structured hospital food facility consisting of a
kitchen, a delivery system, and an ordering system. Grade of recommendation GPP – consensus
(89.5% agreement)
每家医院应建立医院食品设施,包括厨房、递送系统和订餐系统。推荐等级GPP -同意(89.5%)
推荐3
Clear responsibilities for hospital food production and delivery are
necessary for all areas of food supply (ward, kitchen, delivery). Grade of
recommendation GPP – strong consensus (98.3% agreement)
所有食品供应区域(病房,厨房,配送链)都必须明确医院食品生产和交付的责任。推荐等级GPP -强烈同意(98.3%)
推荐4
Hospitals, rehabilitation centers, and nursing homes should aim to use
high-quality and sustainable food ingredients and to avoid food waste as much
as possible. Grade of recommendation GPP – strong consensus (100.0% agreement)
医院、康复中心和疗养院应以使用高质量和可持续的食品原料为目标,尽可能避免食物浪费。推荐等级GPP -强烈同意(100.0%)
推荐5
Patient and personnel surveys regarding hospital food and diets should be
performed on a regular basis, at a minimum once a year. Grade of recommendation
GPP –consensus (90.0% agreement)
应定期对患者和工作人员进行关于医院食品和饮食的调查,至少每年一次。推荐等级GPP -同意(90.0%)
推荐6
Hospital food ordering should be structured, documented, and protocoled.
Grade of recommendation GPP – strong consensus (95.0% agreement)
医院食品订购应结构化、文件化和标准化。推荐等级 GPP – 强烈同意(95.0%)
推荐7
The prescription of hospital food should be performed through the
computerized patient medical record. Grade of recommendation GPP – strong
consensus (92.3% agreement)
医院食品的处方应通过电子病历系统来执行。推荐等级GPP -强烈同意(92.3%)
推荐8
Each hospital, rehabilitation center, or nursing home should propose a
minimal number of two different regular diets (the standard and the hospital
diets) and a minimal number of two different additional diets, adapted to the
size and the focus of the hospital. Grade of recommendation GPP – consensus
(79.6% agreement)
每家医院、康复中心或疗养院都应该根据医院的规模和特色,提出最少两种不同的常规饮食(标准饮食和医院饮食)和最少两种不同的额外饮食。推荐等级GPP -同意(79.6%)
推荐9
Therapeutic diets should be only used if medically indicated. Otherwise, a
regular diet should be used. Grade of recommendation GPP – strong consensus
(100.0% agreement)
仅在有医学指征时才使用治疗性饮食,否则应常规饮食。推荐等级GPP -强烈同意(100%)
推荐10
Diets based on food restriction without medical evidence (e.g. anticancer
starvation) should be avoided in hospitals, because they increase the risk of
malnutrition. Grade of recommendation GPP – strong consensus (97.5% agreement)
医院应避免在没有医学证据的情况下施行限制性饮食(如饥饿抗癌),因为限制性饮食会增加营养不良的风险。推荐等级GPP -强烈同意(97.5%)
推荐11
Hospital food diets should be re-evaluated every three to five years
according to novel data in nutritional sciences and medicine, but also according
to the hospital's focus and needs. Grade of recommendation GPP – consensus
(89.3% agreement)
根据营养学和医学的最近数据以及医院的重点和需求,每三到五年重新评估一次医院的饮食。推荐等级GPP -同意(89.3%)
推荐12
Hospital nutrition should be checked, re-evaluated, and eventually adapted
for each patient at regular intervals (every three to five days) according to
the course of the disease, monitored oral intake, and the patient’s acceptance.
If dietary modifications are insufficient to cover energy and protein needs,
medical nutrition should be provided according to the stage of the disease. For
details, see other ESPEN guidelines and evidence herein. Grade of
recommendation GPP – strong consensus (94.9% agreement)
根据疾病病程、口服摄入量和患者的接受情况,每隔3到5天定期检查、重新评估住院患者的营养状况,并对每位患者进行调整。如果改变饮食不足以满足能量和蛋白质的需求,则应根据疾病阶段提供医学营养治疗。医学营养治疗的详细信息可参阅ESPEN其他指南和证据。推荐等级GPP -强烈同意(94.9%)
二、医院标准饮食
推荐13
The hospitalized patients without or at low nutritional risk and who do not
require special diets should be provided with the standard diet, as advised for
the general population. The indication of this diet should be re valuated after
three to five days. Grade of recommendation GPP – strong consensus (90.9%
agreement)
对于没有营养风险或营养风险较低且不需要特殊饮食的住院患者,应按照一般人群的建议提供标准饮食。这种饮食的适应证应在3到5天后重新评估。推荐等级GPP –强烈同意(90.9%)
推荐14
Hospitalized patients at moderate/high nutritional risk or malnourished
shall be provided with the hospital diet, a protein-energy enriched diet. Grade
of recommendation A – strong consensus (94.2% agreement)
对于中等/高营养风险或营养不良的住院患者,应提供医院饮食,即富含蛋白质和能量的饮食。推荐等级A –强烈同意(94.2%)
推荐15
The standard diet should cover the minimal energy needs (25 kcal/kg actual
BW/day) and the minimum of protein needs (0.8-1.0 g/kg actual BW/day). The
hospital diet should cover 30 kcal/kg actual BW/day of energy needs, and at
least 1.2 g/kg actual BW/day of protein needs. Grade of recommendation GPP –
consensus (86.8% agreement)
标准饮食应包括最低能量需求(25 kcal/kg实际体重/天)和最低蛋白质需求(0.8-1.0 g/kg实际体重/天)。医院饮食应包括30 kcal/kg实际体重/天的能量需求,以及至少1.2 g/kg实际体重/天的蛋白质需求。推荐等级GPP –同意(86.8%)
推荐16
The proportions of carbohydrates, lipids, and protein over the total daily
energy intake should be 50-60 %, 30-35 %, and 15-20 % for the standard diet,
and 45-50%, 35-40%, and 20% for the hospital diet. Grade of recommendation GPP
– majority agreement (69.2% agreement)
标准饮食中碳水化合物、脂类和蛋白质占每日总能量摄入的比例应分别为50-60%、30-35%和15-20%,医院饮食应分别为45-50%、35-40%和20%。推荐等级GPP –多数同意(69.2%)
推荐17
Hospitalized patients should be offered at least two menu choices for each
main meal, lunch, and dinner. Grade of recommendation GPP – strong consensus
(92.2% agreement)
住院患者每顿正餐、午餐和晚餐至少应提供两种菜单选择。推荐等级GPP –强烈同意(92.2%)
三、医院食品配送标准
推荐18
Systematic “between-meals snacks” shall be offered and consumed to reach
nutritional requirements as a standard hospital food service, and prevent night
fasting. Grade of recommendation A – strong consensus (96.2% agreement)
作为标准的医院食品服务,应提供“餐间零食”以达到营养需求,并防止夜间禁食。推荐等级A -强烈同意(96.2%)
推荐19
At least one dietitian working in collaboration with the professionals
involved in the field (e.g. nutrition support team, dietetic department, cooks,
food engineers, food manager) should be dedicated to the hospital kitchen with
the role of setting up patients’ menus according to the different available
diets. Grade of Recommendation GPP – strong consensus (96.2% agreement)
医院厨房应配备至少一名与专业人员(如营养支持小组、饮食部门、厨师、食品工程师、食品经理)合作的营养师,根据不同的饮食设置患者的菜单。推荐等级GPP -强烈同意(96.2%)
推荐20
Hospital food delivery must be adapted to patient’s abilities and perspectives (acute care, rehabilitation unit, palliative
care). Grade of Recommendation GPP – strong consensus (92.3% agreement)
医院提供的食物必须根据患者的能力和情况(急诊护理、康复护理、姑息治疗)进行调整。推荐等级GPP –强烈同意(92.3%)
推荐21
The mealtime should be protected with a time slot reserved for meals. Grade
of Recommendation B – strong consensus (94.6% agreement)
应设置专门的时间段以保证用餐。推荐等级B –强烈同意(94.6%)
四、标准饮食的个例
4.1 食物过敏或食物不耐受是否应考虑到饮食的组成?
推荐22
In patients with proven food allergies, the food allergen shall be excluded
from the patient’s hospital food choice and delivery. Grade of recommendation
GPP – strong consensus (97.4% agreement)
被证实有食物过敏的患者,应将这些食物过敏原排除在该患者的食物选择和供给之外。推荐等级GPP -强烈同意(97.4%)
4.2 在构成标准饮食时,是否应考虑纯素饮食、宗教信仰、食物偏好、可能的食物不耐受等因素?
推荐23
Religious beliefs and food preferences (taste) should be taken into account
at best when proposing the menu choice to the patient. Grade of recommendation
GPP – strong consensus (92.1% agreement)
在向患者建议菜单选择时,最好考虑到宗教信仰和食物偏好(口味)。推荐等级GPP -强烈同意(92.1%)
推荐24
Vegetarian diets shall be designed to cover the energy and protein
requirements (see recommendations 14&15). Grade of recommendation GPP
–consensus (89.4% agreement)
素食主义者的饮食应满足能量和蛋白质的需求(见建议14和15)。推荐等级GPP -同意(89.4%)
推荐25
A vegan diet should not be offered at the hospital. Grade of recommendation
B –consensus (76.5% agreement)
医院不应该提供纯素饮食。推荐等级B -同意(76.5%)
五、治疗性饮食适应证
5.1 去除麸质、可发酵低聚糖/单糖/双糖/多元醇(低FODMAP饮食)和乳糖有什么功效?
推荐26
A gluten-free diet shall be provided to patients with proven celiac
disease. Grade of recommendation A – strong consensus (100.0% agreement)
已证实麸质过敏的患者应提供无麸质饮食。推荐等级A -强烈同意(100.0%)
推荐27
For individuals with irritable bowel syndrome, a diet low in fermentable
oligo-, di-, monosaccharides, and polyols (low FODMAP diet) should be
recommended to improve symptoms including abdominal pain and bloating and to
increase the quality of life. Grade of recommendation B – strong consensus
(91.8% agreement)
对于肠易激综合征患者,推荐的饮食应含较低的可发酵低聚糖/单糖/双糖/多元醇(低FODMAP饮食),以改善腹痛和腹胀等症状,并提高生活质量。推荐等级B -强烈同意(91.8%)
推荐28
A diet low in lactose (<12 g per meal) shall be provided to patients
with proven lactose intolerance (lactose breath test). Grade of recommendation
A – strong consensus (91.8% agreement)
经乳糖呼吸试验证实有乳糖不耐症的患者应提供低乳糖饮食(每餐<12克)。推荐等级A -强烈同意(91.8%)
5.2 高能量饮食和/或高蛋白饮食的指征是什么?
推荐29
The hospital diet should be provided in the hospital setting to be served
to malnourished patients, patients at risk for malnutrition, and other specific
patient groups with a higher need for energy and/or protein. Grade of
recommendation B– strong consensus (92.6% agreement)
医院饮食应在医疗环境中提供给营养不良、有营养风险的患者,以及其他对能量和/或蛋白质有较高需求的特定患者群体。推荐等级B -强烈同意(92.6%)
推荐30
The specifically designed hospital diet should be provided at the hospital
because reaching the energy and/or protein target can hardly be realized with
meals and snacking from the standard diet. Grade of recommendation B– strong
consensus (92.0% agreement)
医院应提供专门设计的医院饮食,因为通过标准饮食中的膳食和零食很难达到目标能量和/或蛋白量。推荐等级B
-强烈同意(92.0%)
5.3 医院采用低热量饮食(减肥饮食)的适应证是什么?
推荐31
Hypocaloric diets are usually not indicated at the hospital and should be
avoided because they increase the risk of malnutrition even in acute care obese
patients. Grade of recommendation B – strong consensus (94.6% agreement)
低热量饮食在医院里通常应该避免,即使是肥胖患者的急性疾病,因为它们增加了营养不良风险。推荐等级B -强烈同意(94.6%)
推荐32
There are very few indications for low-calorie diets in the hospital setting
but they temporally can be indicated in refeeding syndrome, obesity with severe
insulin resistance, and in rehabilitation units for obesity. Grade of
recommendation 0 – strong consensus (91.9% agreement)
医院里的低卡路里饮食适应证非常少,但它们可临时用于再喂养综合征、伴有严重胰岛素抵抗的肥胖患者和肥胖康复中心的患者。推荐等级0 -强烈同意(91.9%)
推荐33
In low-calorie diets, the protein content may not be reduced and may be at
least 1 g/kg actual BW/day if BMI is below 30, and at least 1 g/kg adjusted
BW/day if BMI is ≥30. Grade of recommendation 0 – consensus (85.7% agreement)
低卡路里饮食中,蛋白质含量可能不会降低,如果BMI<30,蛋白质含量至少为1 g/kg实际体重/天,如果BMI≥30,蛋白质含量至少为1
g/kg校正体重/天。推荐等级0 -同意(85.7%)
5.4 低蛋白质饮食的指征是什么?
来自ESPEN肝病临床营养指南的建议
Protein intake should not be restricted in cirrhotic patients with hepatic
encephalopathy as it increases protein catabolism. Grade of recommendation B –
strong consensus (100% agreement)
肝硬化肝性脑病患者不应限制蛋白质摄入,因为它会增加蛋白质分解代谢。推荐等级B -强烈同意(100%)
ESPEN肾病临床营养指南的建议
Chronic kidney disease patients previously maintained on controlled protein
intake (the so-called “low protein diet”) should not be maintained on this
regimen during hospitalization if acute illness is the reason for
hospitalization. Grade of recommendation GPP – strong consensus (100%
agreement)
如果慢性肾病患者因急症住院,住院期间不应继续维持入院前的控制性低蛋白质饮食。推荐等级GPP -强烈同意(100%)
5.5 低脂饮食的指征是什么?
推荐34
Patients with a proven chyle leakage should receive a diet low in
long-chain triglycerides (LCT, <5% of total energy intake) and enriched in
medium-chain triglycerides (MCT, >20% of total energy intake). Grade of
recommendation B – strong consensus (95.7% agreement)
乳糜漏患者应接受低长链甘油三酯(LCT,<总能量摄入的5%)和高中链甘油三酯(MCT,>总能量摄入的20%)饮食。推荐等级B -强烈同意(95.7%)
推荐35
Patients with rare fatty acid oxidation disorders, such as long-chain
3-Hydroxyacil-CoA Dehydrogenase
Deficiency (LCHADD, MIM 609016) and Mitochondrial Trifunctional Protein
Deficiency (MTPD, MIM 609015) and Very Long-Chain Acyl-CoA Dehydrogenase
Deficiency (VLCADD, MIM 201475) should receive a diet low in LCT (<5% of
total energy intake) and enriched in MCT (>20% of total energy intake).
Grade of Recommendation 0 – strong consensus (92.3% agreement)
患有罕见脂肪酸氧化疾病的患者,如长链3-羟基酰基辅酶a脱氢酶缺乏症(LCHADD, MIM 609016)、线粒体三功能蛋白缺乏症(MTPD, MIM 609015)和极长链酰基辅酶a脱氢酶缺乏症(VLCADD, MIM 609015),MIM 201475) 应接受低LCT(<总能量摄入的5%)和高MCT(>总能量摄入的20%)的饮食。推荐等级0 -强烈同意(92.3%)
推荐36
Some cases of intestinal lymphangiectasia with protein-losing enteropathy
should receive a diet low in LCT (<5% of total energy intake) and enriched
in medium-chain triglycerides (>20% of total energy intake). Energy and
protein intakes should be at least 30 kcal/ kg actual BW/day and 1.2 g/kg
actual BW/day. Grade of Recommendation 0 – consensus (89.1% agreement)
一些肠淋巴管扩张伴蛋白丢失性肠病患者应接受低LCT(<总能量摄入的5%)和富含中链甘油三酯(>占总能量摄入的20%)的饮食。能量摄入应至少为30 kcal/ kg实际体重/天,蛋白质摄入应至少为1.2 kcal/ kg实际体重/天。推荐等级0 -同意(89.1%)
5.6 粒细胞缺乏饮食的指征是什么?
推荐37
Neutropenic diets (also called “germ-free”, “no microbial” or “sterilized”
diets) shall not be used (e.g. in neutropenic patients with cancer including
hematopoietic cell transplant patients). Grade of recommendation A – strong
consensus (93.6% agreement)
不应使用粒细胞缺乏饮食(也称为“无菌”、“无微生物”或“灭菌”饮食)(例如患有中性粒细胞减少的癌症患者,包括接受造血干细胞移植的患者)。推荐等级A -强烈同意(93.6%)
5.7 低纤维饮食的指征是什么?
推荐38
Solely on the day preceding a colonoscopy a low fiber diet should be eaten
to achieve a better colon cleansing and to reduce patients’ discomfort. Grade
of recommendation B – strong consensus (94.3% agreement)
仅在结肠镜检查的前一天吃低纤维饮食,以达到更好的结肠清洁和减少患者不适。建议等级B -强烈同意(94.3%)
六、低盐饮食
推荐39
In the case of chronic cardiac failure, chronic renal failure, or
cirrhosis, sodium chloride reduction should not be decreased below 6 g/day,
otherwise, the benefits-risk ratio is
unfavorable towards a higher risk for malnutrition.
Grade of recommendation B – strong
consensus (91.2% agreement)
在慢性心力衰竭、慢性肾衰竭或肝硬化的情况下,氯化钠不应减少至低于6 g/天,否则,获益-风险比趋向于高营养不良风险。推荐等级B -强烈同意(91.2%)
推荐40
In case of arterial hypertension or acute decompensated heart failure,
sodium chloride (salt) intake shall be no more than 6 g per day. Grade of
recommendation B – strong consensus (91.8% agreement)
高血压、急性失代偿性心力衰竭患者,每日氯化钠(盐)摄入量不超过6 g。推荐等级B –强烈同意(91.8%)
推荐41
In patients admitted for acute decompensated heart failure, sodium should
not be restricted to < 120 mmol/day (i.e. 2.8 g sodium chloride per day).
Grade of recommendation B – strong consensus (93.5% agreement)
对于急性失代偿性心力衰竭患者,钠摄入不应限制在<120 mmol/天(即2.8 g氯化钠/天)。推荐等级B –强烈同意(93.5%)
七、特殊患者的饮食
7.1 治疗性饮食是否与皮质类固醇治疗相关?
推荐42
Patients treated with a short-term (≤6 weeks) systemic corticosteroid
therapy may receive the hospital diet (see recommendation 14). Grade of recommendation
0 – consensus (87.8% agreement)
进行短期(≤6周)系统性皮质类固醇治疗的患者可给予医院饮食(见建议14)。推荐等级0 -同意(87.8%)
7.2 糖尿病患者有推荐的饮食吗?
推荐43
Type 1 and 2 diabetic patients should be offered the standard or the
hospital diet according to their nutritional risk/status (see recommendations
12,13,14). Grade of recommendation GPP –consensus (84.0% agreement)
1型和2型糖尿病患者应根据其营养风险/状况提供标准饮食或医院饮食(见推荐12,13,14)。推荐等级GPP -同意(84.0%)
推荐44
Patients with insulin therapy shall receive support to identify and
quantify their dietary carbohydrate intake for glycemic control. Grade of
recommendation A – strong consensus (97.1% agreement)
应帮助接受胰岛素治疗的患者确定和量化他们的碳水化合物摄入量,以控制血糖。推荐等级A -强烈同意(97.1%)
推荐45
Snacks containing mixed carbohydrates and protein should be offered between
meals according to individual care (e.g. usually with mealtime short- and
median-acting insulin) and glycemic control. Grade of recommendation GPP
–consensus (89.4% agreement)
应根据个人治疗(例如通常使用短效和中效胰岛素)和血糖控制情况,在两餐之间提供混合碳水化合物和蛋白质的零食。推荐等级GPP -同意(89.4%)
推荐46
In hospitalized diabetic patients, the low carbohydrate diet (<40% of
energy intake) should be avoided as it is associated with lower energy intake
and the risk of malnutrition. Grade of recommendation GPP – strong consensus
(91.8% agreement)
住院的糖尿病患者应避免低碳水化合物饮食(<能量摄入的40%),因为它与较低的能量摄入和营养不良风险相关。推荐等级GPP -强烈同意(91.8%)
推荐47
With diabetic complications (e.g. diabetic nephropathy, diabetic
gastroparesis, lower limb ulcers, and amputations), diet and nutrition support
should be individual and diagnosis-based. Grade of recommendation GPP – strong
consensus (97.3% agreement)
对于糖尿病并发症(如糖尿病肾病、糖尿病胃轻瘫、下肢溃疡和截肢),应基于具体情况给予个体化的饮食和营养支持。推荐等级GPP -强烈同意(97.3%)
八、调整饮食质地
8.1 更改饮食质地的适应证
ESPEN指南对老年患者临床营养和水合作用的建议
Older persons with malnutrition or at risk of malnutrition and signs of oropharyngeal
dysphagia and/or chewing problems shall be offered texture-modified, enriched
foods as a compensatory strategy to support adequate dietary intake. Grade of
recommendation GPP – strong consensus (100 % agreement)
对于营养不良或存在营养风险以及有吞咽困难和/或咀嚼问题的老年患者,应提供改良质地、营养丰富的食物,以支持适当的膳食摄入。推荐等级GPP –强烈同意(100%)
8.2 改良饮食除老年病学外的其他适应证?
推荐48
In clinical situations at risk of dysphagia (stroke, neurogenic and
neuromuscular disorders, head and neck
cancer, amyotrophic lateral sclerosis, hereditary ataxia, multiple sclerosis,
or traumatic cervical spinal cord injury), systematic screening of dysphagia
should be performed, and the need and type of modified texture diet should be
identified. Grade of recommendation GPP – strong consensus (91.7% agreement)
对于存在吞咽困难风险的患者(中风、神经源性和神经肌肉疾病、头颈癌、肌萎缩性侧索硬化症、遗传性共济失调、多发性硬化症或外伤性颈脊髓损伤),应进行吞咽困难的系统筛查,并确定改良食物质地的需求和种类。推荐等级GPP -强烈同意(91.7%)
推荐49
In the initial stages of dysphagia, adequate nutrition intake may be
achieved through dietary modification to include soft, semisolid, or
semi-liquid consistencies, in combination with appropriate swallowing
techniques. Grade of recommendation GPP – strong consensus (97.3% agreement)
在吞咽困难的最初阶段,可以通过改变饮食,包括软的、半固体的或半液体的稠度,结合适当的吞咽技术来获得足够的营养摄入。推荐等级GPP -强烈同意(97.3%)
九、营养恢复流程
9.1 急性胰腺炎后营养恢复的推荐流程是什么?
ESPEN指南对急、慢性胰腺炎临床营养的建议
Oral feeding shall be offered as soon as clinically tolerated and
independent of serum lipase concentrations in patients with predicted mild
acute pancreatitis. Grade of recommendation A – strong consensus (100%
agreement)
对于预测为轻度急性胰腺炎的患者,应在临床耐受的情况下尽快给予口服营养,无需参考血清脂肪酶浓度。推荐等级A –强烈同意(100%)
ESPEN指南对急、慢性胰腺炎临床营养的建议
Low-fat, soft oral diet shall be used when reinitiating oral feeding in
patients with mild acute pancreatitis. Grade of recommendation A – strong
consensus (100% agreement)
轻型急性胰腺炎患者重新开始口服时应使用低脂、软性口服饮食。推荐等级A –强烈同意(100%)
ESPEN指南关于急、慢性胰腺炎临床营养的声明
Patients with chronic pancreatitis do not need to follow a restrictive
diet. strong consensus (94% agreement)
慢性胰腺炎患者不需要限制性饮食。强烈同意(94%)
ESPEN指南对急、慢性胰腺炎临床营养的建议
Chronic pancreatitis patients with a normal nutritional status should
adhere to a well-balanced diet. Grade of recommendation GPP – strong consensus
(94% agreement)
营养状况正常的慢性胰腺炎患者应坚持均衡饮食。推荐等级GPP –强烈同意(94%)
ESPEN指南对急、慢性胰腺炎临床营养的建议
Malnourished patients with chronic pancreatitis should be advised to
consume high protein, high-energy food in five to six small meals per day.
Grade of recommendation GPP – strong consensus (94% agreement)
建议营养不良的慢性胰腺炎患者每天5到6次小餐中食用高蛋白、高能量的食物。推荐等级GPP –强烈同意(94%)
ESPEN指南对急、慢性胰腺炎临床营养的建议
In patients with chronic pancreatitis, diets very high in fiber should be
avoided. Grade of recommendation B – strong consensus (91% agreement)
慢性胰腺炎患者应避免高纤维饮食。推荐等级B –强烈同意(91%)
ESPEN指南关于急、慢性胰腺炎临床营养的声明
In patients with chronic pancreatitis, there is no need for dietary fat
restriction unless symptoms of steatorrhea cannot be
controlled. strong consensus (100% agreement)
在慢性胰腺炎患者中,除非脂肪泻症状无法控制,否则没有必要限制脂肪摄入。强烈同意(100%)
9.2 胃肠手术(除肥胖手术)后营养恢复的推荐流程是什么?
推荐50
Small meals five to six times per day may help patients to tolerate oral
feeding and achieve nutritional goals faster during the early phase of recovery
after surgery. Grade of recommendation GPP – strong consensus (94.3% agreement)
在术后恢复的早期阶段,每天5 – 6次小餐可以帮助患者耐受口服喂养,更快地实现营养目标。推荐等级GPP –强烈同意(94.3%)
ESPEN外科临床营养指南
In most instances, oral nutritional intake shall be continued after surgery
without interruption. Grade of recommendation A – strong consensus (90 %
agreement)
大多数情况下,术后应继续口服营养摄入,不得中断。推荐等级A –强烈同意(90%)
ESPEN外科临床营养指南
It is recommended to adapt oral intake according to individual tolerance
and to the type of surgery carried out with special caution to elderly
patients. Grade of recommendation GPP – strong consensus (100 % agreement)
建议根据个体的耐受性和所进行的手术类型来调整口服营养,对老年患者需特别小心。推荐等级GPP –强烈同意(100%)
ESPEN外科临床营养指南
Oral intake, including clear liquids, shall be initiated within hours after
surgery in most patients. Grade of recommendation A – strong consensus (100 %
agreement)
大部分患者应在术后数小时内开始口服,包括清流质。推荐等级A –强烈同意(100%)
9.3 下消化道或上消化道出血(溃疡、食管静脉曲张)后推荐的营养恢复流程是什么?
推荐51
After lower gastrointestinal bleeding, once oral food is authorized,
patients should receive the standard hospital diet according to the patient
nutritional risk and status. Grade of recommendation GPP – strong consensus
(91.8% agreement)
下消化道出血后,一旦确定可以经口进食,应根据患者的营养风险和状况接受标准的医院饮食。推荐等级GPP –强烈同意(91.8%)
推荐52
After upper gastrointestinal system bleeding, once oral food is authorized,
oral feeding should be initiated with liquids and advanced within 24 hours to
standard or hospital diet according to the patient nutritional risk and status.
Grade of recommendation B – strong consensus (93.8% agreement)
上消化道出血后,一旦确定可以经口进食,应先开始口服液体,并根据患者的营养风险和状况在24小时内进展到标准或医院饮食。推荐等级B级–强烈同意(93.8%)
9.4 内镜检查(包括胃造口介入手术)后的营养恢复流程是什么?
推荐53
Patients undergoing an endoscopic procedure should return to a standard
hospital diet after the release of medication (anesthesia) to prevent
malnutrition risk during hospitalization. Grade of recommendation GPP – strong
consensus (97.3% agreement)
接受内窥镜手术的患者在药物(麻醉)恢复后应恢复标准的医院饮食,以防止住院期间出现营养不良风险。推荐等级GPP –强烈同样(97.3%)
10 其他
10.1 是否需要组合饮食?
推荐54
The combination of therapeutic diets may not be prescribed, as the risk of
insufficient food intake and malnutrition is high. Grade of recommendation 0 –
strong consensus (91.4% agreement)
不能将治疗性饮食进行组合,因为这会导致食物摄入不足和营养不良的发生风险增加。推荐等级0 –强烈同意(91.4%)
10.2如何以及何时评估医院食物摄入量?
推荐55
Food intake is part of nutritional assessment and should be monitored by
semi-quantitative methods at hospital admission, at least every week during the
hospital stay in patients with no nutritional risk, and every day in patients
with nutritional risk or malnourished. Grade of recommendation B – strong
consensus (96.1% agreement)
食物摄入量是营养评估的一部分,在入院时应采用半定量方法监测,无营养风险的患者住院期间至少每周监测一次,有营养风险或营养不良的患者住院期间应每天监测一次。推荐等级B –强烈同意(96.1%)
推荐56
In nutritionally at-risk patients, insufficient food intake equal to or
less than 50% of energy requirements over 3 days during the hospital stay
should trigger a nutritional intervention. Grade of recommendation B – strong
consensus (94.1% agreement)
存在营养风险的患者,入院后食物摄入量不能达到50%的能量需求超过3天,应启动营养干预。推荐等级B –强烈同意(94.1%)
作者:吴国豪 谈善军 张燕妮 王俊杰
编辑:谈善军 张知格
审核:吴国豪

